Question for Physiotherapists

Gout
Welcome to Orthosports Question for Physiotherapists April 2024. This month Dr John Negrine discusses the common condition of Gout.
SAVE THE DATE: Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, live @UNSW or via webinar.
If you have a Question that you would like answered on this monthly email please send to education@orthosports.com.au

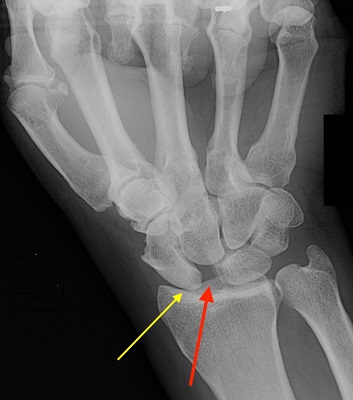
QUESTION | A 63 year old man presents with pain in the left forefoot intermittently. The pain is in the region of his second MTP joint, it is not necessarily activity related. He presents with forefoot swelling. His initial xrays were reported as normal but…
The diagnosis is usually obvious but not always. Paradoxically the serum uric acid may fall during an acute attack which can confound the diagnosis.
Aspirating a red hot joint and sending the fluid for examination under polarised light will confirm the diagnosis (the needle shaped crystals are strongly negatively birefringent).
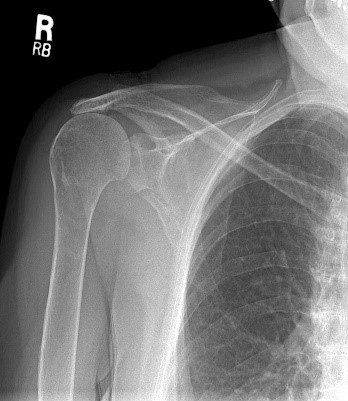
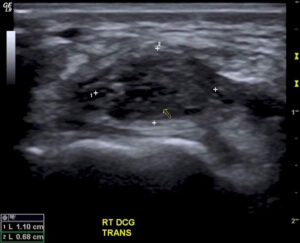
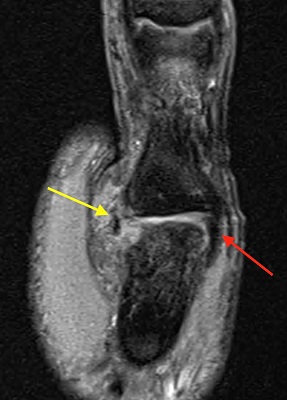
The case below illustrates an atypical presentation and a new method of making the diagnosis non-invasively.
The patient has a pacemaker and can’t have an MRI.


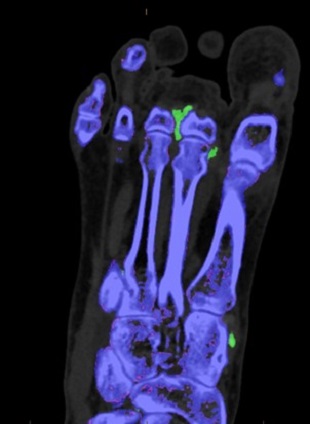
Take home message: Dual energy CT scan is a relatively new non-invasive test for gout with very high sensitivity and specificity. False negatives can occur however in the setting of acute recent onset gout. False positives can occur in patients with advanced knee arthritis.
Distal Biceps Rupture
Welcome to Orthosports Question for Physiotherapists February 2024. This month Dr Doron Sher discusses management of distal biceps rupture. If you have a Question that you

Sport after Total Knee Replacement
Welcome to Orthosports Question for Physiotherapists, October 2023. This month Dr Doron Sher discusses return to sport after total knee replacement. REMINDER: Register your place for the Annual Orthopaedic Updates.

High Tibial Osteotomy and Uni Knee Replacement
Welcome to Orthosports Question for Physiotherapists, September 2023. This month Dr Doron Sher discusses the comparison of the High Tibial Osteotomy vs the Unicompartmental Knee Replacement. Register your
Achilles Tendon Ruptures
Welcome to Orthosports Question for Physiotherapists, August 2023. This month Dr John Negrine discusses Achilles Tendon Ruptures. Save the Date: Saturday, 4th November, 2023 Annual Orthopaedic Updates. Live

Lateral extra-articular tenodesis
Welcome to Orthosports Question for Physiotherapists, June 2023. This month Dr Michael Goldberg discusses lateral extra-articular tenodesis and why you would add this procedure to an ACL
Adding a Patch to Rotator Cuff Repairs
Welcome to Orthosports Question for Physiotherapists, May 2023. This month Dr Doron Sher discusses the use of a patch in Rotator Cuff Repairs. Save the Date: Saturday, 4th

Imaging for ACL Injury
Welcome to Orthosports Question for Physiotherapists, October 2022. This month Dr Doron Sher discusses imaging for a suspected ACL injury. Save the Date: Saturday, 12 November, 2022 Annual
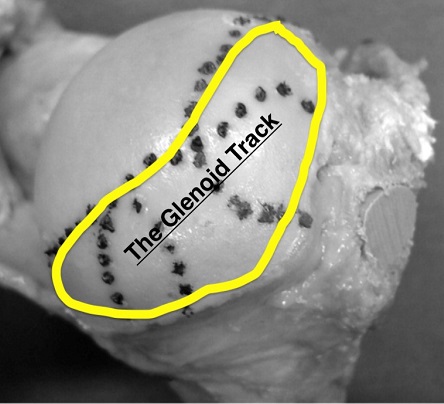
Glenoid Track and Shoulder Instability
Welcome to Orthosports Question for Physiotherapists August, 2022. This month Dr Doron Sher discusses a question on the glenoid track and shoulder instability. Save the Date: Saturday,

OSTEOCHONDRITIS DISSECANS
Welcome to Orthosports Question for Physiotherapists May, 2022. This month Dr Doron Sher discusses a question on treatment options for an OCD Lesion. Save the Date: Saturday,
Accessory Bones of the Foot and Ankle
Welcome to Question for Physiotherapists, April, 2022 This month Dr John Negrine discusses accessory bones of the foot and ankle. Please feel free to send your

Hypermobile Lateral Meniscus
Welcome to Question for Physiotherapists, March, 2022 This month Dr Michael Goldberg discusses the Hypermobile Lateral Meniscus. Please feel free to send your questions to

Imaging in Musculoskeletal assessment
Welcome to Question for Physiotherapists, February, 2022 This month Dr Paul Annett discusses Imaging inMusculo-skeletal Assessment. Please feel free to send your questions to education@orthosports.com.au Dr
Shoulder Injury related to vaccine administration
Welcome to Question for Physiotherapists, January, 2022 This month Dr Doron Sher discusses Shoulder Injury related to Vaccine administration. Please feel free to send your questions

Chondral Grafting in the knee
Welcome to Question for Physiotherapists, November 2021. This month Dr Doron Sher discusses Chondral Grafting in the knee.Please feel free to send your questions to education@orthosports.com.au CHONDRAL

Syndesmosis Fixation
Welcome to Question for Physiotherapists, October 2021. This month Dr Todd Gothelf discusses Syndesmosis fixation. Please feel free to send your questions to education@orthosports.com.au QUESTION I

Hip Precautions following Total Hip Replacement
Welcome to Question for Physiotherapists, September 2021. This month Dr Christopher Spelman discusses precautions after a Total Hip Replacement. Please feel free to send your questions
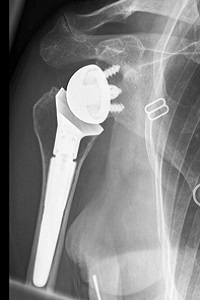
Reverse Shoulder Replacement Rehabilitation
Welcome to Question for Physiotherapists, August 2021. This month Dr Doron Sher discusses rehabilition after a Reverse Shoulder Replacement. Please feel free to send your questions
Chronic Scapholunate Ligament Rupture
Welcome to Question for Physios, July 2021. This month Dr Kwan Yeoh discusses the management of Complete Scapholunate Ligament Rupture. Please feel free to send your

Assessing Sports Injury
Welcome to Question for Physiotherapists June 2021. This month Dr Paul Annett presents an article on assessing a patient that presents with potentially more than a

Discoid Lateral Meniscus
Welcome to Question for Physiotherapists May 2021. This month Dr Doron Sher presents an article on a Discoid Lateral Meniscus. Please feel free to send

Cavo-Varus (High Arched) Feet
QUESTION | Why are high arched feet more interesting than flat feet? ANSWER | A 43 year old man presents with numbness on the outer

Surgical Treatment of Unstable Shoulder
QUESTION | | Surgical treatment of the unstable shoulder – How do you decide which patient gets what operation? We know that younger patients and those
Full Thickness Tear of Supraspinatus Tendon
QUESTION | My patient is a 67 year old female who has had pain during overhead activity (catching pain), going on for over 5 years.

Medial Meniscal Root Tears
QUESTION I I have a patient in her 50s who has had a meniscus repair done. I thought that the studies showed no advantage when doing
Wrist Ganglion & Carpal Instability
QUESTION| How Does a Wrist Ganglion relate to Carpal Instability? How is it best treated? ANSWER | A ganglion is a benign synovium-lined cystic collection of

Lumbar Stress Fractures
QUESTIONS | 1. What is rest in treatment of stress fracture? Walking only? Bike? Swim(in non-extended position)? What can you do? Or is it just not
Collateral Ligament Tear
QUESTION | WHEN DOES A COLLATERAL LIGAMENT TEAR OF THE THUMB NEED SURGERY? ANSWER | For the purposes of this question, I’m going to assume
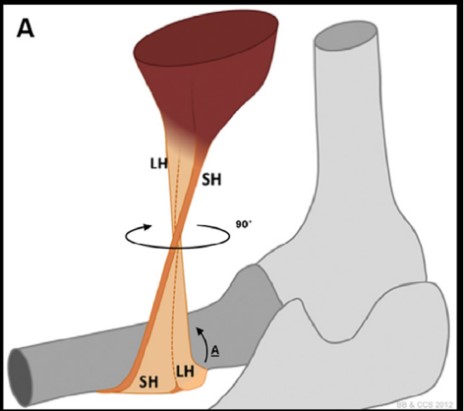
Distal Biceps Rupture
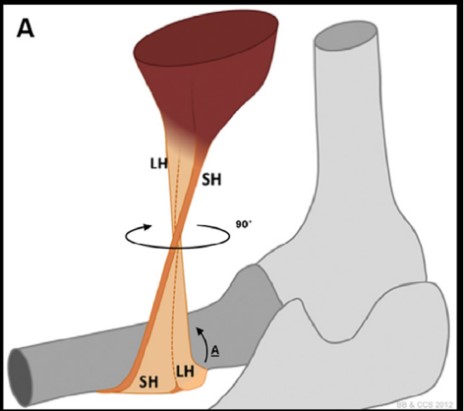
QUESTION | I recently had a patient with a partial distal biceps rupture. Why was he offered surgery without trying non-operative management? ANSWER | Anatomy:

Hallux Rigidus
QUESTION | What are the best options for a 50 year old runner with Hallux Rigidus? ANSWER | A 50 year old runner with hallux
Previous Question for Physiotherapists:
| Dec-2020 | Wrist Ganglions | Dr Kwan Yeoh |
| Oct/Nov-2020 | Medial Meniscal Root Tears | Dr Doron Sher |
| Sep-2020 | Lumbar Stress Fractures | Dr Paul Annett |
| Aug-2020 | Frailty and Healthy Ageing | Dr John Best |
| Jul-2020 | Thumb – Collateral Ligament Tear | Dr Kwan Yeoh |
| Jun-2020 | Shoulder Instability | Dr Doron Sher |
| May-2020 | Hallux Rigidus | Dr John Negrine |
| Mar/Apr-2020 | Achilles Tendon Ruptures | Dr Todd Gothelf |
| Feb-2020 | Distal Biceps | Dr Doron Sher |
| Nov-2019 | Clavicle Fracture Internal Fixation | Dr Doron Sher |
| Oct-2019 | Femoracetabular Impingement (FAI) | Dr Paul Mason |
| Sep-2019 | Imaging for Acute ACL Injuries | Dr Doron Sher |
| Aug-2019 | Joint Relocation | Dr Paul Annett |
| Jul-2019 | Guyon canal surgery | Dr Kwan Yeoh |
| Jun-2019 | Whats new in ACL reconstruction 2019 | Dr Doron Sher |
| May-2019 | Cuneiform Fracture | Dr Todd Gothelf |
| Apr-2019 | Flexor Tendon Injuries | Dr Kwan Yeoh |
| Mar-2019 | Chronic Exertional Compartment Synd | Dr Paul Annett |
| Feb-2019 | Achilles Tendon Rupture | Dr John Negrine |
| Nov-2018 | Low Back Pain | Dr Paul Mason |
| Sep-2018 | Concussion part 2 | Dr John Best |
| Jul-2018 | Concussion part1 | Dr Paul Annett |
| Jun-2018 | Thessaly & McMurray Test | Dr Doron Sher |
| May-2018 | AC Joint | Dr Doron Sher |
| Apr-2018 | Arthritis of the fingers | Dr Kwan Yeoh |
| Feb-2018 | CLAVICLE fractures | Dr Doron Sher |
| Oct-2017 | ACL Grafts | Dr Doron Sher |
| Sep-2017 | Forefoot pain | Dr John Negrine |
| Aug-2017 | Wrist Ganglion | Dr Kwan Yeoh |
| Jul-2017 | Anterolateral Ligament Reconstruction | Dr Doron Sher |
| Jun-2017 | Scapholunate ligament | Dr Kwan Yeoh |
| Apr-2017 | Knee Brace – ACL Reconstruction | Dr Doron Sher |
| Mar-2017 | Sesamoid fractures | Dr Kwan Yeoh |
| Feb-2017 | Plantar Fasciitis | Dr Todd Gothelf |
| Nov-2016 | Sternoclavicular Joint | Dr Doron Sher |
| Oct-2016 | Proximal Humerus Fractures | Dr David Lieu |
| Sep-2016 | Wrist Fractures | Dr Kwan Yeoh |
| Aug-2016 | Patella Instability | Dr Doron Sher |
| Jul-2016 | Snowboarders ankle | Dr Todd Gothelf |
| May-2016 | Cortisone Injections | Dr Paul Annett |
| Apr-2016 | Shoulder Instability_1 | Dr Ivan Popoff |
| Mar-2016 | Exercise after TKR | Dr Doron Sher |
| Dec-2015 | Scaphoid OA | Dr Kwan Yeoh |
| Nov-2015 | Greater Tuberosity Fractures | Dr Doron Sher |
| Oct-2015 | Stress Fractures | Dr Paul Annett |
| Sep-2015 | Boxers Fractures | Dr Kwan Yeoh |
| Aug 2015 | Resistance Training | Dr John Best |
| July 2015 | LARS Ligament | Dr Ivan Popoff |
| Jun-2015 | Distal Biceps | Dr Doron Sher |
| May-2015 | Latarjet procedure | Dr Jerome Goldberg |
| Apr-2015 | TFCC Questions | Dr Kwan Yeoh |
| Mar-2015 | Acute Ankle Sprains | Dr Todd Gothelf |
| Nov-2014 | PRPP | Dr Paul Annett |
| Oct-2014 | Driving After Surgery | Dr Doron Sher |
| Sep-2014 | Distal Biceps Rupture | Dr Doron Sher |
| Aug-2014 | Ankle Sprain | Dr Todd Gothelf |
| Jun-2014 | Patella Dislocation | Dr Doron Sher |
| May-2014 | Shoulder Instability | Dr Todd Gothelf |
| Apr-2014 | De Quervains | Dr Kwan Yeoh |
| Mar-2014 | Acromio-clavicular joint injuries | Dr Todd Gothelf |
| Feb-2014 | Chronic Knee Pain | Dr Paul Annett |
| Dec-2013 | Foot and Ankle Questions | Dr John Negrine |
| Oct-2013 | Rotator Cuff Repair | Dr Todd Gothelf |
| Sep-2013 | ACL Reconstruction | Dr Doron Sher |
| Jul-2013 | Slipped Upper femoral epiphysis | Dr Rod Pattinson |
| May-2013 | Skiers thumb | Dr Kwan Yeoh |
| Apr-2013 | Bakers_Cyst | Dr Ivan Popoff |
| Mar-2013 | Tibial Osteotomy vs UKR | Dr Doron Sher |
| Feb-2013 | ALIF success rate | Dr Andreas Loefler |
| Jan-2013 | Lisfranc Injuries | Dr Todd Gothelf |
| Nov-2012 | Anterior Spinal Fusions | Dr Andreas Loefler |
| Oct-2012 | MCL Injuries | Dr Doron Sher |
| Sep-2012 | Compartment Syndrome | DrPaul Annett |
| Aug-2012 | Carpal tunnel | Dr Kwan Yeoh |
| July-2012 | Anterior Process Calcaneus Fx | Dr Todd Gothelf |
| Jun-2012 | Tenodesis vs Tenotomy | DrJeromeGoldberg |
| May-2012 | Osteoarthritis in the young active patient | Dr Doron Sher |
| Apr-2012 | Syndesmosis Sprain | Dr Todd Gothelf |
| Mar-2012 | Triangular Fiocartilage Injuries | Dr Kwan Yeoh |
| Jan-2012 | Shoulder Replacement Older Population | Dr Jerome Goldberg |
| Dec-2011 | Wrist Fracture | Dr Kwan Yeoh |
| Nov-2011 | Adductor Tendon Tear | Dr Paul Annett |
| Oct-2011 | Navicular Pain | Dr Todd Gothelf |
| Sep-2011 | OCD Lesion | Dr Doron Sher |
| Aug-2011 | Metal on Metal Hip Replacements | Dr Andreas Loefler |
| July-2011 | Femoral Neck Stress Fract (Pt 2) | Dr John Best |
| Jun-2011 | Femoral Neck Stress Fractures | Dr John Best |
| May-2011 | PCL Injury Part 2 | Dr Doron Sher |
| Apr-2011 | PCL Injury Part 1 | Dr DoronSher |
| Mar-2011 | Prolotherapy Autologous Blood Injections | DrPaul Annett |
| Feb-2011 | Shoulder Impingement | Dr Todd Gothelf |
| Dec-2010 | Does Chondral Grafting Work | DrDoron Sher |
| Nov-2010 | Shoulder Immobilisation-Dislocation | Dr Jerome Goldberg |
| Sep-2010 | SLAP Lesions Stable Shoulder | Dr ToddGothelf |
| Jul-2010 | Ankle Sprains | Dr Todd Gothelf |
| Jun-2010 | Dislocation After THR | Dr Peter Walker |
| May-2010 | Acupuncture Muscle Strength Programmes | Dr Paul Annett |
| April-2010 | Full Thickness Rotator Cuff Tears | Dr JeromeGoldberg |
| Mar-2010 | Skiing after TKR | Prof Warwick Bruce |
| Feb-2010 | Fractures of the Clavicle | Dr John Trantalis |
| Jan-2010 | Osteoarthritis of the Knee | Dr Doron Sher |
| Dec-2009 | Fifrth Metatarsal Fractures | Dr Todd Gothelf |
| Nov-2009 | Partial Rotator Cuff Tears | Dr Todd Gothelf |
